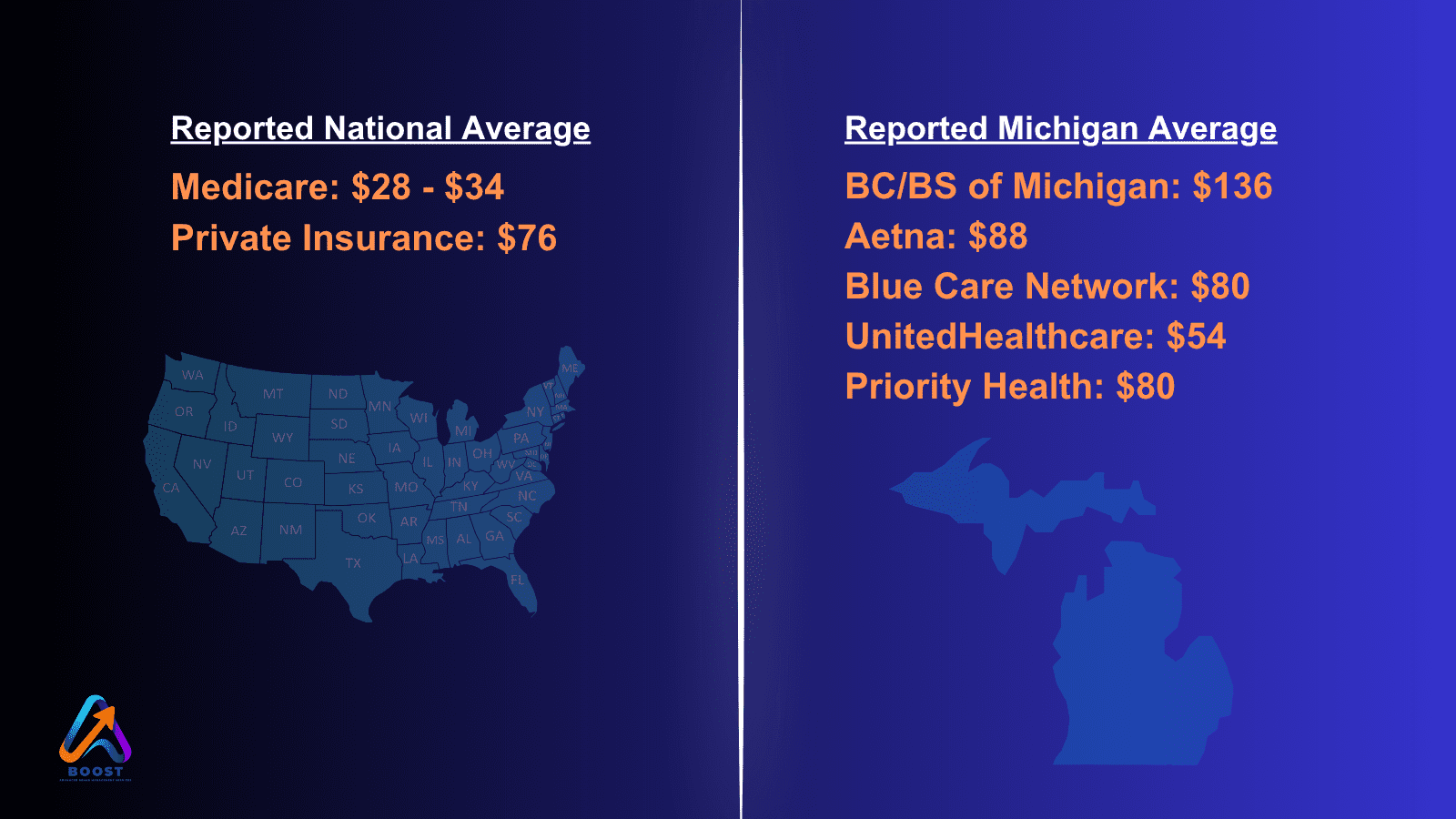
Wouldn’t it be nice if reimbursements were standard and as a Physical Therapist, you knew exactly how much the insurance company would pay for certain treatments? As a provider, you can negotiate a contract, but those agreed-upon prices depend on your location and the specific treatment codes you use.
For
example:
Workers' Comp & Auto Claims
When it comes to workers’ comp and auto injury claims, Physical Therapy owners are often surprised when insurance companies use PPO, Retroactive and Network Deductions to pay less for the care their clinic provides. The reimbursements are often lower than even the negotiated contract price.
Physical Therapy owners across 27 states have found a way to BOOST their reimbursements by $53 per visit, getting the payments they deserve. Payments are higher and more consistent with BOOST and they don’t have to overhaul their systems or add extra work.
Reimbursement Reductions COming
This year, Medicare implemented a 2.93% reduction in payment
rates for Physical Therapy. That reduction follows 4 straight years of cuts. Private
Insurance rates have dropped 10% in the past decade and are expected to stay
the same or drop in 2025.
BOOSt My Claims
The BOOST Processing Method is the solution to declining reimbursements for Workers' Compensation and MVA (motor vehicle accident) bills. Since 2014, they've successfully employed this method to enhance profits for Physical Therapy Clinic owners. It's a well-established approach that can seamlessly integrate into your current billing process. With BOOST, you can get 2x higher reimbursements and generate. To see if you qualify: boostmyclaims.com
